|
|
Periodontal DIseases Periodontal Disease is a bacterial infection of the gums, bone and ligaments that
support the teeth and anchor them in the jaw. The bacteria are normal inhabitants of the mouth and form a film of dental plaque
and calculus (tartar) which stick to the teeth. The bacteria produce poisonous toxins which stimulate the immune response
to fight the infection. If the disease process is not stopped, the supporting structures of the teeth will continue to be
destroyed. This eventually leads to tooth loss. Periodontal disease can occur at any age. Over half of all
people over the age of 18 have some form of the disease. After age 35, over 75% of all people are affected. Unfortunately,
the disease process is usually asymptomatic and painless. The disease can be easily detected during regular dental examinations. The most common type of periodontal disease are GINGIVITIS
and PERIODONTITIS
|
||
|
GINGIVITIS is infection
of the gingiva (gum tissue), and is the initial stage of the disease process. Gums become red, swollen and may bleed easily.
Underlying bone levels are unaffected. PERIODONTITIS is classified
as being Mild, Moderate or Severe, depending upon the amount of destruction to the gums, ligaments and bone that surround
teeth. As the disease progresses, gums separate from the teeth and form gum pockets. These pockets get deeper as more underlying
bone is destroyed. Gum pockets will collect increasing amounts of bacterial plaque and calculus (tartar) as the disease process
worsens. Teeth will loosen as more bone is lost. Lower teeth -SEVERE PERIODONTITIS
- Upper teeth
CONTRIBUTING FACTORS TO PERIODONTAL DISEASE The response of the gums and bone to dental plaque
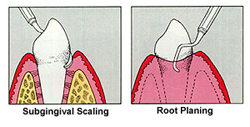
may be modified by one or more of the following factors. WARNING SIGNS OF PERIODONTAL DISEASE DIAGNOSIS OF PERIODONTAL DISEASE TREATMENT OF PERIODONTAL DISEASE Scaling and root planing are performed to clean the tooth structure and remove bacterial
plaque and calculus deposits (the source of the infection) from the gum pockets. This may be the only treatment necessary
in cases of gingivitis and very mild periodontitis.
|
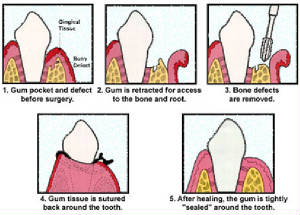
PHASE II
Additional treatment modalities may be necessary to treat
periodontal disease and restore health. These may include: MAINTENANCE |
|
|
|
||